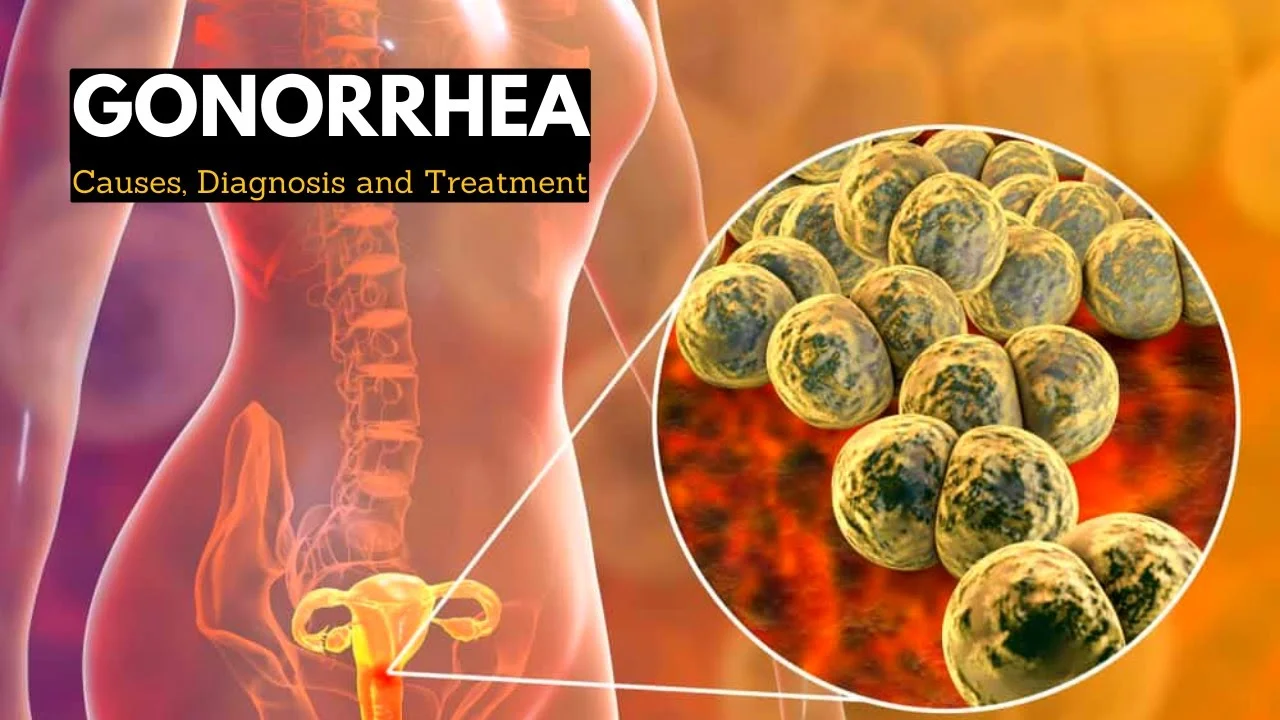
Gonorrhea is one of the most common sexually transmitted infections (STIs) worldwide, affecting millions of people each year. Despite its prevalence, many remain uninformed about its causes, symptoms, and treatment options. This comprehensive guide provides everything you need to know about gonorrhea, from recognizing early warning signs to effective prevention strategies.
What Is Gonorrhea? Understanding the Basics

Gonorrhea is a bacterial infection caused by Neisseria gonorrhoeae (also called gonococcus), which primarily affects the mucous membranes of the reproductive tract. It can infect the cervix, uterus, and fallopian tubes in women, and the urethra, prostate, and epididymis in men. The infection can also develop in the rectum, throat, and eyes.
Often referred to as “the clap” in colloquial terms, gonorrhea spreads primarily through sexual contact with an infected person. According to the Centers for Disease Control and Prevention (CDC), gonorrhea is the second most commonly reported bacterial STI in the United States, with approximately 820,000 new infections occurring annually.
The History and Origin of Gonorrhea
Gonorrhea has affected humans for centuries, with descriptions of symptoms dating back to ancient medical texts:
- The earliest documented references appear in the Bible and in Chinese medical texts from 2600 BCE
- Galen, a prominent Greek physician, named the condition in 130 CE, using the term “gonorrhea” (meaning “flow of seed”)
- Albert Neisser identified the causative bacterium (Neisseria gonorrhoeae) in 1879
- Before antibiotics, various treatments were used, including silver nitrate and mercury compounds
- The first effective treatment, sulfonamides, was introduced in the 1930s, followed by penicillin in the 1940s
Throughout history, gonorrhea has been a significant public health concern, with its impact fluctuating with changes in social behavior and medical advances.
Common Symptoms of Gonorrhea: What to Watch For
One of the challenging aspects of gonorrhea is that many infected individuals—especially women—may not develop noticeable symptoms. This “silent” nature contributes to its spread, as people may unknowingly transmit the infection to others.
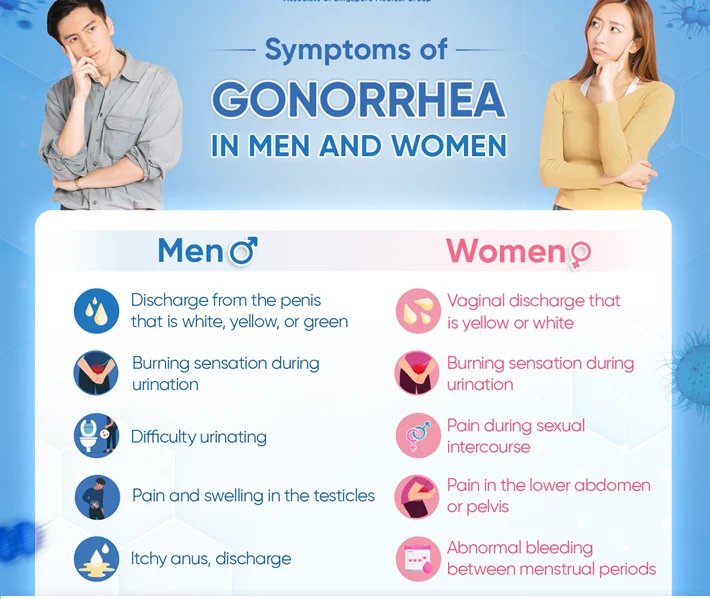
Symptoms in Women
- Abnormal vaginal discharge that may be yellow or greenish
- Burning or pain during urination
- Increased vaginal bleeding between periods
- Pain during sexual intercourse
- Lower abdominal or pelvic pain
- Sore throat (if infection is in the throat)
- Rectal pain, discharge, or bleeding (if infection is in the rectum)
Many women mistake these symptoms for a bladder or vaginal infection. Approximately 50-80% of women with gonorrhea may not experience noticeable symptoms in the early stages.
Symptoms in Men
- White, yellow, or green discharge from the penis
- Burning or pain during urination
- Painful or swollen testicles (less common)
- Sore throat (if infection is in the throat)
- Rectal pain, discharge, or bleeding (if infection is in the rectum)
Men are more likely to experience symptoms than women, with approximately 90% developing noticeable signs within 2-14 days after infection.
Gonorrhea in Other Body Parts
- Rectal infections: Pain, discharge, bleeding, and itching
- Eye infections: Conjunctivitis (pink eye), sensitivity to light, and discharge
- Throat infections: Sore throat and swollen lymph nodes, though often asymptomatic
- Disseminated gonococcal infection: Joint pain, skin rashes, and fever when the bacteria spread through the bloodstream
How Gonorrhea Spreads: Transmission and Risk Factors
Understanding how gonorrhea spreads is crucial for prevention:
Primary Transmission Methods
- Vaginal sex: The most common route of transmission
- Anal sex: Can lead to rectal infections
- Oral sex: Can cause throat infections
- Mother to baby: During childbirth, potentially causing serious eye infections
The bacteria cannot survive long outside the human body, so you cannot get gonorrhea from toilet seats, swimming pools, or sharing food.
High-Risk Groups
While anyone who is sexually active can contract gonorrhea, certain factors increase risk:
- Age: People under 25 have higher rates of infection
- Previous gonorrhea infection: Having had gonorrhea before increases the risk of reinfection
- Multiple sexual partners: More partners means increased exposure risk
- Inconsistent condom use: Proper and consistent condom use significantly reduces risk
- Men who have sex with men (MSM): Higher prevalence exists in this community
- Sex workers and their clients: Due to multiple partners and potential inconsistent protection
Complications of Untreated Gonorrhea: Long-term Health Risks
When left untreated, gonorrhea can lead to serious health complications:
Complications in Women
- Pelvic Inflammatory Disease (PID): Infection of the reproductive organs that can cause chronic pelvic pain
- Infertility: Scarring of the fallopian tubes increases the risk of infertility
- Ectopic pregnancy: Higher risk of dangerous pregnancies developing outside the uterus
- Chronic pelvic pain: Long-term discomfort that may persist even after treatment
About 10-15% of women with untreated gonorrhea develop PID, and of those, about 15% will become infertile.
Complications in Men
- Epididymitis: Inflammation of the epididymis (tube that carries sperm), causing pain and swelling
- Prostatitis: Inflammation of the prostate gland
- Urethral stricture: Narrowing of the urethra due to scarring
- Rare cases of infertility: Usually reversible with prompt treatment
Systemic Complications
- Disseminated gonococcal infection (DGI): When the bacteria enter the bloodstream and spread throughout the body
- Arthritis: Inflammation and pain in joints due to infection
- Endocarditis: Infection of the heart valves (rare)
- Meningitis: Inflammation of the membranes covering the brain and spinal cord (rare)
Increased HIV Risk
Individuals with gonorrhea have an increased risk of contracting HIV if exposed. The inflammation caused by gonorrhea makes it easier for HIV to enter the bloodstream.
Diagnosis: How Gonorrhea Is Detected
Early and accurate diagnosis is essential for effective treatment:
Testing Methods
- Nucleic Acid Amplification Tests (NAATs): The most common and accurate tests that detect the bacterium’s genetic material
- Gram stain: Microscopic examination of discharge samples (more commonly used for men)
- Culture tests: Growing the bacteria in a lab environment (useful for antibiotic resistance testing)
- Urine tests: Non-invasive option that can detect the infection
Who Should Get Tested?
The CDC recommends annual testing for:
- Sexually active women under 25
- Women over 25 with new or multiple partners
- Men who have sex with men (at sites of possible exposure)
- People with HIV
- Anyone with symptoms or whose partner has been diagnosed with gonorrhea
Effective Treatments for Gonorrhea: Medical Approaches
Gonorrhea is curable with the right antibiotics, though treatment has become more challenging with antibiotic resistance:

Current Treatment Recommendations
The CDC currently recommends:
- Dual therapy: Ceftriaxone (injection) plus azithromycin (oral) as the first-line treatment
- Alternative regimens: For patients with allergies or in areas with different resistance patterns
Treatment should begin immediately after diagnosis, even before test results if infection is strongly suspected.
Antibiotic Resistance Concerns
Gonorrhea has developed resistance to nearly all antibiotics used for treatment:
- Penicillin resistance emerged in the 1970s
- Fluoroquinolone resistance became widespread by 2007
- Cephalosporin resistance is now a growing concern
The CDC monitors resistance patterns through the Gonococcal Isolate Surveillance Project (GISP).
Post-Treatment Guidelines
- Abstain from sexual activity for 7 days after completing treatment
- Partners should be treated to prevent reinfection
- Get retested 3 months after treatment to ensure the infection is cleared
- HIV testing is recommended for all individuals diagnosed with gonorrhea
Partner Notification: An Essential Step in Treatment
Partner notification is crucial for breaking the chain of transmission:
- All recent sexual partners (within the past 60 days) should be notified
- Many clinics offer anonymous partner notification services
- Expedited Partner Therapy (EPT) allows providers to give patients medications to deliver to their partners in some states
Studies show that proper partner notification can reduce reinfection rates by up to 68%.
Home Remedies and Supportive Care: Managing Symptoms
While antibiotics are essential for treating gonorrhea, some home remedies may help manage symptoms:
Supportive Measures (Not Replacements for Medical Treatment)
- Pain management: Over-the-counter pain relievers like ibuprofen or acetaminophen
- Warm baths: May help relieve pelvic or testicular discomfort
- Loose clothing: To reduce friction and irritation
- Adequate hydration: Drinking plenty of water to help flush the urinary system
- Probiotics: May help restore vaginal flora after antibiotic treatment
Important Warning
No home remedy, herbal treatment, or supplement can cure gonorrhea. Attempting to treat gonorrhea without antibiotics can lead to serious complications and increase the risk of spreading the infection to others.
Prevention Strategies: Protecting Yourself and Others
Prevention remains the best approach to gonorrhea:
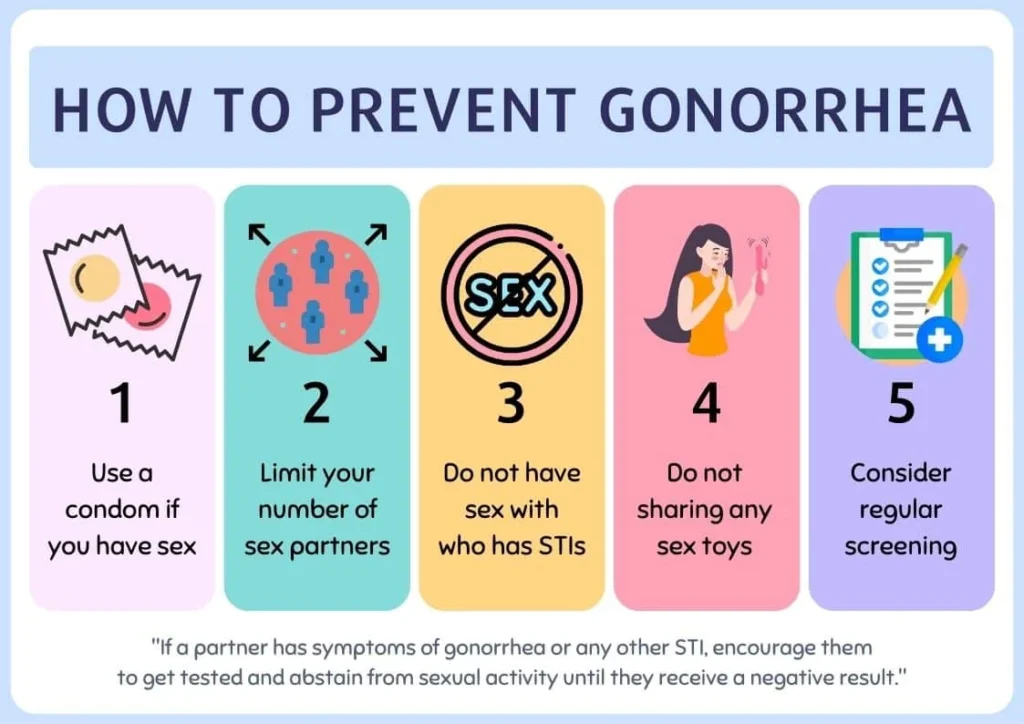
Safe Sex Practices
- Consistent and correct condom use: Male condoms reduce the risk of transmission by approximately 70-80%
- Dental dams: For protection during oral sex
- Regular testing: For sexually active individuals, especially those with multiple partners
- Mutual monogamy: With a partner who has tested negative
- Communication: Open discussions about STI status with partners
Specific Prevention Tips
- Get vaccinated: While there’s no gonorrhea vaccine yet, getting vaccinated against other STIs like HPV and hepatitis B reduces overall sexual health risks
- Avoid douching: This practice can alter the natural balance of bacteria in the vagina
- Consider pre-exposure measures: If you’re at high risk, discuss regular testing schedules with your healthcare provider
- Recognize high-risk activities: Understand that unprotected oral, anal, and vaginal sex all carry transmission risks
Gonorrhea in Special Populations
Certain groups require special consideration for gonorrhea prevention and treatment:
Pregnant Women
- Screening is recommended at the first prenatal visit
- Untreated gonorrhea can lead to premature birth and low birth weight
- Newborns can develop serious eye infections (ophthalmia neonatorum)
- Safe treatment options exist during pregnancy
HIV-Positive Individuals
- Higher risk of gonorrhea transmission and acquisition
- May experience more severe symptoms
- Treatment follows the same guidelines but with closer monitoring
- Regular screening is especially important
Adolescents and Young Adults
- Account for half of all new STI cases
- May face barriers to testing and treatment due to confidentiality concerns
- Many states allow minors to consent to STI services without parental knowledge
Living with Gonorrhea: Emotional and Social Aspects
Being diagnosed with gonorrhea can have psychological impacts:
- Stigma management: Understanding that STIs are common and not a reflection of character
- Disclosure discussions: How to inform current and future partners
- Emotional support: Resources for coping with diagnosis
- Healthcare relationship: Maintaining open communication with healthcare providers
Support groups, online forums, and counseling services can provide assistance for those struggling with the emotional aspects of diagnosis.
Global Impact and Epidemiology of Gonorrhea
Gonorrhea affects populations worldwide:
- The WHO estimates 87 million new cases globally each year
- Rates are highest in the Western Pacific Region and Africa
- In the United States, rates have increased by 63% since 2014
- Disproportionately affects racial minorities and low-income communities
- Rising resistance threatens treatment efficacy globally
Research and Future Directions in Gonorrhea Management
Several promising developments may change how we approach gonorrhea:
Vaccine Development
- Multiple vaccine candidates in various stages of research
- Challenges include the bacteria’s ability to change surface proteins
- A successful vaccine could dramatically reduce global prevalence
New Antibiotics
- Several new antibiotics in clinical trials
- Zoliflodacin and gepotidacin show promise against resistant strains
- Combination therapy approaches being studied
Rapid Point-of-Care Testing
- New diagnostic tools that provide results in minutes instead of days
- Could allow for immediate treatment and reduce transmission
When to Seek Medical Help: Warning Signs
Prompt medical attention is important if you:
- Experience symptoms consistent with gonorrhea
- Have been exposed to someone with gonorrhea
- Notice new or unusual discharge, pain, or discomfort in genital areas
- Experience fever, rash, or joint pain after potential exposure
- Have concerns about any sexual health matter
Most healthcare providers, urgent care centers, and sexual health clinics can provide testing and treatment.
Conclusion: Taking Control of Your Sexual Health
Gonorrhea is a common but preventable and treatable infection. By practicing safe sex, getting regular testing, and seeking prompt treatment when necessary, you can protect yourself and your partners. Remember that sexual health is an important component of overall wellness, and there should be no shame in seeking information, testing, or treatment.
If you suspect you may have gonorrhea or any other STI, contact a healthcare provider promptly. With early detection and proper treatment, the risk of complications can be significantly reduced.
Frequently Asked Questions About Gonorrhea
Q: Can gonorrhea go away on its own?
No, gonorrhea requires antibiotic treatment to clear the infection. Without treatment, it can persist for months or years and lead to serious complications.
Q: How quickly does gonorrhea show up after exposure?
Symptoms typically appear 2-14 days after exposure in men who develop symptoms. Women often don’t develop noticeable symptoms.
Q: Can you get gonorrhea from kissing?
No, gonorrhea cannot be transmitted through casual contact such as kissing, hugging, sharing food, or touching surfaces.
Q: Is gonorrhea curable?
Yes, gonorrhea is curable with the right antibiotics. However, treatment cannot repair any permanent damage caused by the infection.
Q: Can I get gonorrhea again after being treated?
Yes, having gonorrhea once does not make you immune. You can be reinfected if exposed to the bacteria again.
Q: Does using condoms prevent gonorrhea?
Consistent and correct use of condoms significantly reduces but doesn’t completely eliminate the risk of gonorrhea transmission.
Q: Can I still have children if I’ve had gonorrhea?
Most people who receive prompt treatment for gonorrhea can still have children. However, if PID or other complications develop before treatment, fertility may be affected.
Q: Is gonorrhea testing part of routine STI screening?
Not always. Many providers don’t automatically test for gonorrhea unless requested or if you have symptoms or risk factors. Always discuss which infections you’re being tested for.
ALSO READ MORE HEALTH ARTICLES FROM CHIID HEALTH