In today’s image-conscious world, children face unprecedented pressures regarding their appearance and body size. The dual challenges of promoting positive body image while preventing unhealthy weight gain require thoughtful, balanced approaches from parents, educators, and healthcare providers. This comprehensive guide explores evidence-based strategies that support both physical health and emotional wellbeing in young people, creating foundations for lifelong healthy relationships with food, exercise, and self-perception.
What Is Body Image and Why It Matters for Children

Body image refers to how individuals perceive, think about, and behave toward their own physical appearance. For children and adolescents, body image begins forming early—research suggests awareness of body size and cultural appearance ideals starts as young as age 3-5, with significant development during elementary school years.
A child’s body image exists on a spectrum from positive to negative:
- Positive body image involves acceptance of one’s natural body shape, appreciation for body functionality, and resilience against unrealistic beauty standards.
- Negative body image includes persistent dissatisfaction with appearance, preoccupation with perceived flaws, and feelings of shame or anxiety about one’s body.
The significance of healthy body image in young people cannot be overstated. Research consistently shows that positive body image correlates with:
- Higher self-esteem and confidence
- Better mental health outcomes
- Healthier eating behaviors
- More physical activity participation
- Stronger social relationships
- Greater academic achievement
Conversely, negative body image is associated with increased risk of depression, anxiety, disordered eating, and social withdrawal.
The Origins of Body Image Concerns in Children
Understanding how body image perceptions develop helps identify intervention points for fostering healthier attitudes. Multiple factors influence how children view their bodies:

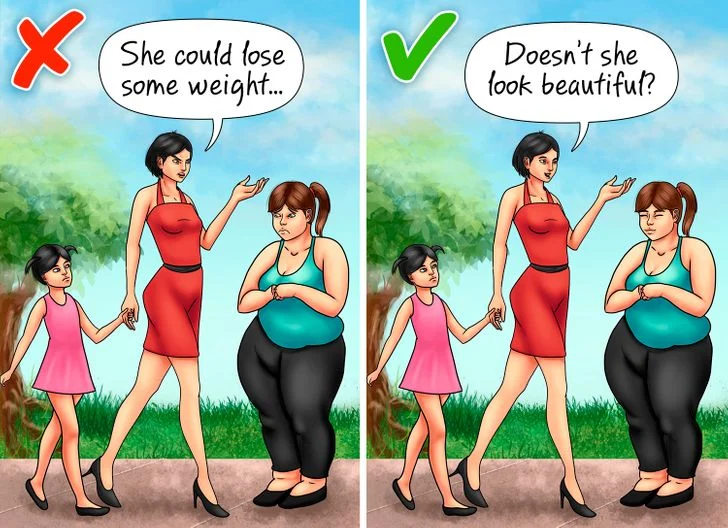
Family Influence
The family environment serves as the primary context for early body image development:
- Parental modeling: Children observe how adults talk about and treat their own bodies
- Direct comments: Casual remarks about weight, appearance, or eating habits can leave lasting impressions
- Family food culture: Attitudes toward eating, dieting, and weight management within the home
- Weight-based teasing: Even “playful” comments about body size can be deeply harmful
Research indicates that children whose parents frequently discuss weight, appearance, or dieting are significantly more likely to develop body dissatisfaction, regardless of their actual body size.
Media and Social Influences
External messaging shapes children’s understanding of “ideal” bodies:
- Traditional media: Television, movies, and magazines often present narrow beauty ideals
- Social media: Platforms expose children to filtered, edited images and appearance-focused content
- Peer interactions: Weight-related teasing and appearance comparisons among friends
- School environment: Athletic competitions, dress codes, and health education approaches
Studies show that media literacy—the ability to critically analyze media messages—can significantly reduce the negative impact of these influences.
Weight Stigma and Bias
Societal attitudes toward weight affect how children view themselves and others:
- Anti-fat bias: Negative assumptions about individuals in larger bodies
- Weight-based bullying: Teasing, exclusion, or harassment based on body size
- Healthcare messaging: How medical professionals address weight concerns
- Educational approaches: How schools implement weight management initiatives
Weight stigma contributes to psychological distress regardless of a child’s actual weight status and can unintentionally reinforce negative body image even when intended to promote health.
The Relationship Between Body Image and Weight
The connection between body image and weight is nuanced and bidirectional:
How Body Image Affects Weight Management
- Motivation: Positive body image provides healthier motivation for self-care behaviors
- Sustainable habits: Body acceptance correlates with more consistent health behaviors
- Emotional eating: Negative body image can trigger comfort eating or food restriction
- Activity participation: Body insecurity may reduce participation in physical activities
Research consistently shows that shame-based approaches to weight management backfire, while acceptance-based approaches lead to more sustainable health behaviors.
How Weight Status Affects Body Image
- Social feedback: Children in larger bodies often experience more appearance-focused comments
- Activity limitations: Weight may affect participation in certain activities, impacting self-perception
- Clothing fit: Difficulty finding age-appropriate clothing can reinforce body dissatisfaction
- Health interventions: Well-intentioned but insensitive approaches to weight concerns
Studies indicate that the emotional impact of weight status often has more to do with social treatment than the weight itself.
Evidence-Based Strategies for Promoting Positive Body Image
Research supports several approaches to fostering healthy body image in young people:
Body Appreciation Focus
- Body functionality: Emphasize what bodies can do rather than how they look
- Body gratitude: Practice thankfulness for specific body capabilities and features
- Body diversity awareness: Teach that bodies naturally come in diverse shapes and sizes
- Body neutrality: Reduce overall focus on appearance in daily conversations
Programs teaching body appreciation show significant improvements in self-esteem and reduced appearance fixation among children.
Media Literacy Development
- Critical analysis skills: Help children question media messages about “ideal” bodies
- Image manipulation awareness: Teach how photos are edited and filtered
- Diverse representation: Expose children to bodies of all types portrayed positively
- Social media boundaries: Establish healthy limits on appearance-focused content
Studies show that even brief media literacy interventions can improve body satisfaction and resilience against appearance pressures.
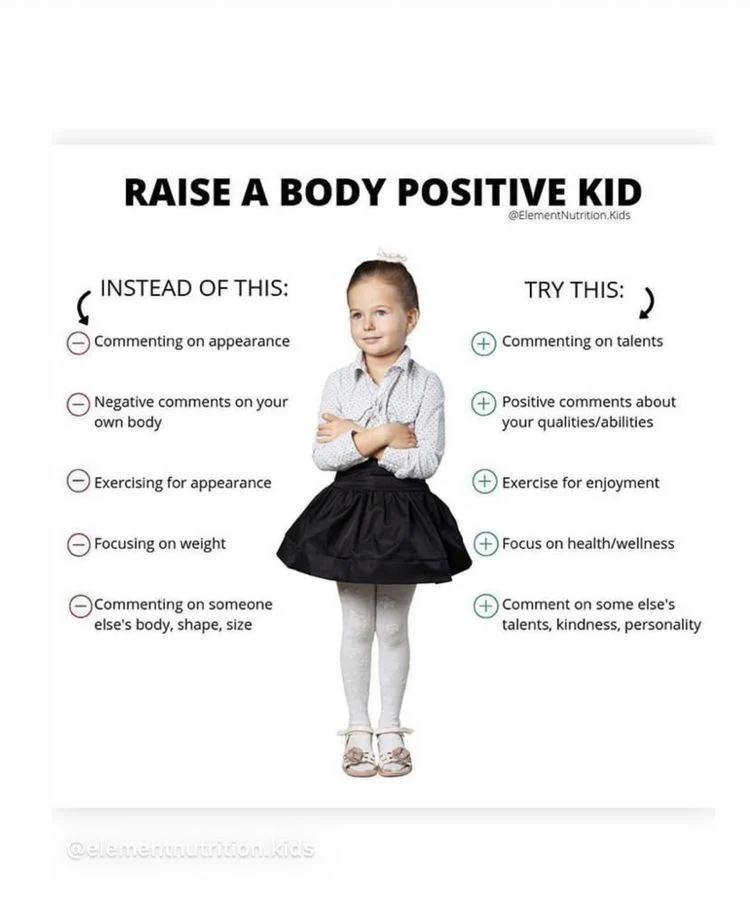
Language Modification
- Body-neutral comments: Avoid appearance-based compliments or criticisms
- Behavior-focused feedback: Comment on actions and choices rather than physical traits
- Weight-neutral terminology: Use non-stigmatizing language around body size
- Health-centered vocabulary: Focus on specific behaviors rather than weight outcomes
Research indicates that eliminating weight-focused language significantly reduces body dissatisfaction and unhealthy weight control behaviors.
Healthy Weight Management: Non-Diet Approaches for Children
Supporting appropriate weight development without harming body image requires careful approaches:
Intuitive Eating Principles
Teaching children to recognize and respond to internal cues supports healthy eating patterns:
- Hunger/fullness awareness: Help children recognize and respond to body signals
- Food neutrality: Avoid labeling foods as “good” or “bad”
- Satisfaction factor: Acknowledge the role of enjoyment in eating
- Body respect: Base food decisions on wellbeing rather than size manipulation
Research shows that intuitive eating practices correlate with better long-term weight outcomes and healthier psychological relationships with food.
Joyful Movement Approaches
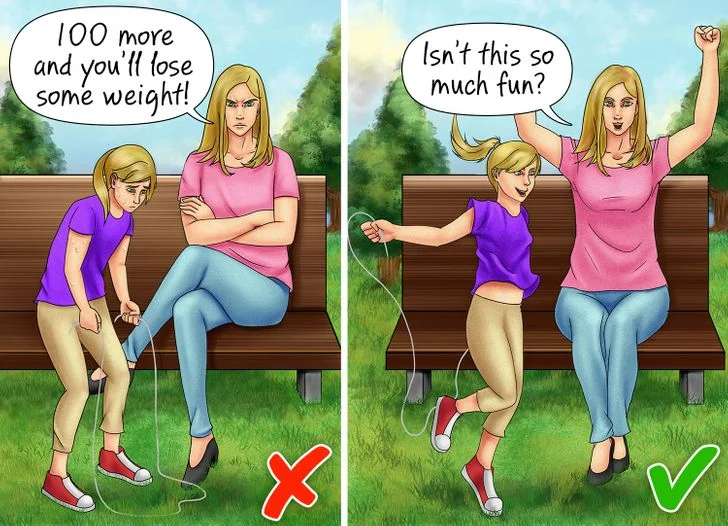
Physical activity supports healthy weight when approached positively:
- Activity exploration: Expose children to diverse movement options
- Pleasure priority: Emphasize enjoyment over calorie-burning
- Competence building: Develop skills that create positive activity experiences
- Social connection: Foster community through group activities
Studies consistently show that enjoyment is the strongest predictor of sustained physical activity in young people.
Family Meal Environment
The context of eating significantly impacts both nutrition and body image:
- Regular shared meals: Establish consistent family eating opportunities
- Positive mealtime atmosphere: Keep conversation pleasant and connection-focused
- Division of responsibility: Parents provide nutritious options; children choose what and how much
- Modeling balanced eating: Demonstrate varied, flexible food choices
Research indicates that family meals correlate with both better nutritional intake and more positive body image in children.
Warning Signs: When Body Image Concerns Require Intervention
Parents and caregivers should remain alert for signs that body image concerns are becoming problematic:
Emotional Red Flags
- Body preoccupation: Excessive discussion of weight, shape, or appearance
- Comparison behaviors: Frequently measuring against peers or media figures
- Negative self-talk: Self-criticism focused on physical appearance
- Body checking: Repeated examination of specific body parts
Behavioral Warning Signs
- Food restriction: Eliminating food groups or significantly reducing intake
- Exercise compulsion: Activity that feels obligatory rather than enjoyable
- Body concealment: Excessive covering of the body regardless of weather
- Social withdrawal: Avoiding activities due to appearance concerns
Early intervention for these warning signs can prevent progression to more serious issues like eating disorders. When observed, consultation with healthcare providers is recommended.
Specialized Approaches: Supporting Body Image in Different Contexts
Certain situations require tailored strategies for body image support:
Athletic Environments
Sports participation provides health benefits but may intensify body image concerns:
- Performance focus: Emphasize capability over appearance
- Weight-neutral coaching: Avoid body composition discussions when possible
- Sport-specific body diversity: Highlight successful athletes with varied body types
- Fueling education: Frame nutrition as performance support rather than weight control
Medical Settings
Healthcare interactions significantly impact how children perceive their bodies:
- Weight-neutral healthcare: De-emphasize BMI and weight measurements
- Respectful examination: Obtain consent and explain procedures
- Sensitive communication: Discuss health concerns without stigmatizing language
- Health-focused goals: Target specific health behaviors rather than weight numbers
School Environments
Educational settings powerfully influence body image development:
- Anti-bullying policies: Explicitly include weight-based teasing in prevention efforts
- Inclusive physical education: Ensure activity options for all ability and comfort levels
- Health curriculum review: Examine messages about weight and bodies in health classes
- Staff training: Educate teachers about weight stigma and body image impacts
Parental Guide: Creating a Body-Positive Home Environment
Parents play a crucial role in fostering positive body image through daily interactions:
Communication Strategies
How adults talk about bodies significantly impacts children’s self-perception:
- Compliment character: Focus praise on non-appearance attributes
- Avoid body comparison: Never compare children’s bodies to others
- Limit appearance comments: Reduce overall focus on how people look
- Model self-acceptance: Demonstrate comfort with your own body
Nutritional Approaches
Food attitudes at home shape lifelong relationships with eating:
- Food variety: Offer diverse options without pressure
- Neutral food language: Avoid “junk food” or “diet food” terminology
- Permission with structure: Set meal schedules but allow choice within options
- Satisfaction emphasis: Acknowledge enjoyment as part of healthy eating
Media Management
Thoughtful media consumption supports healthier body perceptions:
- Content selection: Choose media featuring diverse body types
- Critical viewing: Watch together and discuss unrealistic portrayals
- Limitation without shame: Set reasonable screen time boundaries
- Counter-messaging: Actively challenge narrow beauty standards
Professional Support Options: When to Seek Additional Help
Sometimes professional guidance is beneficial for addressing body image concerns:
Types of Professional Support
- Pediatricians trained in weight-neutral approaches: Medical care without weight stigma
- Child psychologists: Support for body image distress and related anxiety
- Registered dietitians: Non-diet nutrition guidance for families
- Family therapists: Help addressing family dynamics around food and bodies
Finding Appropriate Providers
- Interview questions: Ask potential providers about their approach to weight and body image
- Philosophy alignment: Seek professionals who practice weight-inclusive care
- Credential verification: Ensure appropriate training and specialization
- Communication comfort: Choose providers who communicate respectfully with children
Frequently Asked Questions About Children’s Body Image and Weight
Q: How do I talk to my child about their weight without damaging their body image?
Focus conversations on specific health behaviors rather than weight itself. Instead of discussing body size, talk about how nutritious foods provide energy, how physical activity helps bodies function well, and how sleep supports growth. When weight must be discussed (such as in medical contexts), use neutral language that avoids blame or shame. Emphasize that bodies naturally come in different sizes and that health exists across the weight spectrum. Research shows that behavior-focused rather than weight-focused conversations lead to better outcomes for both physical and mental health.
Q: Is it harmful to encourage my child to lose weight if they’re medically classified as overweight?
Direct weight loss messaging can unintentionally harm children’s body image and relationship with food, even when medically indicated. Instead, experts recommend focusing on gradual, sustainable lifestyle improvements for the entire family without emphasizing weight change as the goal. This might include adding more fruits and vegetables, finding enjoyable physical activities, establishing regular meal times, and limiting screen time. These approaches support appropriate weight development while protecting psychological wellbeing. If weight management is medically necessary, work with healthcare providers who use weight-neutral, non-stigmatizing approaches.
Q: How can I help my child who is being teased about their weight?
First, provide emotional support and validation for your child’s feelings. Help them develop responses to teasing that set boundaries while maintaining self-respect. Teach that body diversity is natural and that worth isn’t determined by appearance. Work with school officials to address bullying through established protocols. Consider finding body-positive community activities where your child can develop confidence and supportive relationships. If teasing causes significant distress, consultation with a child psychologist can provide additional coping strategies. Remember that your home should be a safe haven where your child’s body is never a source of criticism.
Q: At what age should I start being concerned about my child’s body image?
Body image awareness begins surprisingly early, with research showing children as young as 3-5 years old already absorbing cultural messages about “desirable” body types. By age 6, many children express body dissatisfaction and awareness of dieting concepts. Therefore, creating a body-positive environment should begin in early childhood. Watch for signs of body dissatisfaction at any age, such as negative body comments, comparison behaviors, or sudden interest in dieting. Early intervention is most effective, so address concerning behaviors promptly through positive, matter-of-fact conversations about body diversity and health behaviors.
Q: How do I promote healthy eating without creating food issues?
Establish a balanced approach where nutritious foods are provided without rigid control or food moralization. Follow the “division of responsibility” in feeding: parents decide when, where, and what foods are offered; children decide whether and how much they eat from these options. Avoid labeling foods as “good” or “bad,” which can create unnecessary guilt and food preoccupation. Model enjoyment of varied foods yourself, including occasional treats without guilt. Research consistently shows that overly restrictive feeding practices often backfire, leading to increased interest in restricted foods and reduced ability to self-regulate intake.
Q: Can complimenting my child’s appearance harm their body image?
While well-intentioned, frequent appearance-based compliments can unintentionally reinforce the message that looks are highly important and subject to evaluation. This doesn’t mean never commenting positively on appearance, but rather maintaining a balanced focus where physical attributes receive proportionally less attention than character, abilities, and actions. When commenting on appearance, focus on expressions of personality (like a creative outfit choice) rather than features tied to beauty standards. Research indicates that children who receive primarily non-appearance-based compliments develop more resilient body image and stronger self-concept.
Q: How can I help my child who wants to diet?
Express concern about dieting while validating the feelings behind this desire. Explain that restrictive diets often lead to nutritional gaps, reduced energy, and unhealthy relationships with food, especially during growth periods. Redirect toward positive health behaviors that don’t involve restriction, such as adding more fruits and vegetables, finding enjoyable physical activities, and ensuring adequate sleep. If appropriate, discuss media literacy and how images are often manipulated. If dieting preoccupation persists, consider consultation with healthcare providers who specialize in non-diet approaches to child health.
Q: How do I balance teaching healthy habits without creating body insecurity?
Frame healthy behaviors as ways to care for a body that deserves respect rather than methods to change appearance. Focus on immediate benefits of healthy choices (energy, strength, mood improvement) rather than weight outcomes. Avoid connecting health behaviors to appearance or creating a sense that health practices are compensatory or punishing. Emphasize enjoyment in both eating and physical activity. Research shows that intrinsic motivation (doing things because they feel good) leads to more sustainable health behaviors than extrinsic motivation (doing things to change appearance).
Conclusion: Fostering Body Positivity as a Foundation for Lifelong Health
Creating environments where children develop positive body image while maintaining healthy weights requires thoughtful balance. Rather than treating these goals as contradictory, research increasingly shows they are complementary—children with positive body image are more likely to engage in health-promoting behaviors that support appropriate weight development.
The most effective approaches focus on adding positive elements—enjoyable movement, nutritious foods alongside treats, appreciative body relationships—rather than restriction, criticism, or fear-based messaging. By emphasizing capability over appearance, internal cues over external rules, and acceptance over criticism, adults can help children develop relationships with their bodies that support both physical and mental wellbeing.
As our understanding of body image development continues evolving, one conclusion remains consistent: children thrive when they learn that their bodies are instruments for living rather than ornaments for viewing—valuable not for how they look, but for how they allow experience of the world. This foundation of body respect creates resilience against appearance pressures while supporting the health behaviors that allow children to flourish physically, emotionally, and socially throughout their lives.
ALSO READ MORE HEALTH ARTICLES FROM CHIID HEALTH